How to get prior authorization for medical care
Have you ever tried to make an appointment to get a medical test, arrange for a treatment, or fill a prescription from your dermatologist only to find out that you need prior authorization?
When some patients hear these two words, they don’t know what to do next. The following explains what you need to know.
Your health insurance provider may require you to get prior authorization before you fill a prescription or get other medical care.

What is prior authorization?
Prior authorization, also called prior approval or pre-authorization, is a process that many health insurance companies, as well as Medicare and Medicaid, use to manage costs.
Before you can get coverage for certain medications, tests, procedures, surgeries, and medical devices, you need to get prior authorization. Without prior authorization, you may end up paying the entire cost or be denied the treatment.
Who needs to get prior authorization?
What requires prior authorization can vary from one insurance provider to another. It can also vary from plan to plan, year to year, or state to state.
For example, you may be treating a skin condition with a medication that isn’t working as well as you’d like. During your last dermatology appointment, your dermatologist wrote a prescription for a different medication. When you tried to fill the new prescription, your pharmacist told you that you need prior authorization, even though you never needed this for the other medication.
How long does it take to get prior authorization?
Insurance providers typically reply to a request for prior authorization within 30 business days, and many providers could reply sooner. For example, when dermatologists tracked how long it took patients at their practice to get a reply for prior authorization for a biologic medication, they found that about half of their patients had a reply in under 8 business days. Response time varied with the type of medication prescribed.1
Steps for getting prior authorization
While each insurance provider may use slightly different steps, here is what typically happens during the prior authorization process.
Your dermatologist writes a prescription: After your prescription is sent to the pharmacy by your dermatologist or dropped off by you, the pharmacist will run the prescription through your insurance. Then, your insurance company will let either you or someone at your dermatologist’s office know if you need a prior authorization.
What you need to know: What requires prior authorization varies from one health plan to another, so your dermatologist may be unaware that a prescription or test requires prior authorization under your plan. There are hundreds of medications and many health plans.
Some health plans allow you to log in to your member account or patient portal to find out different options, such as whether your plan covers or partially covers your medication, the price, or any limits and requirements. If you learn that you need prior authorization, contact your dermatologist’s office as soon as possible. They have experience getting prior authorization.Your dermatologist’s office creates a request and submits the information required by your insurance provider for prior authorization.
What you need to know: Your dermatologist’s office will let you know what is required of you when requesting prior authorization. You may only need to keep track of updates coming through the patient portal or wait for a call from your dermatologist on a decision.Your insurance provider informs your dermatologist’s office (or you) of its decision. If approved or denied, the following could happen:
- Prior authorization approved: You can fill the prescription, begin the treatment, or schedule the testing that your dermatologist prescribed for you; or
- Prior authorization denied: Someone in your dermatologist's office prepares the materials required to appeal this decision.
What you need to know: Sometimes, the insurance provider tells only the patient of its decision. If your insurance provider contacts you, reach out to your dermatologist’s office to let them know the decision. If the insurance provider denies the request for prior authorization, you can appeal.
If your initial request was denied: Here’s what happens next. Many people feel discouraged when they find out that the insurance provider denied the request for prior authorization. Don’t give up. You have the right to appeal this decision.
Many patients who appeal eventually get approval. For example, dermatologists at one practice found that 64.6% of appeals to get insurance coverage for a prescription were approved.2
What you need to know: You can help the appeal process run more smoothly by staying on top of any paperwork you get about prior authorization and staying in touch with your dermatologist’s office on your progress. In addition to your dermatologist writing an appeal letter for you, it is often helpful to write your own appeal letter to your health insurance to make it more personal.
When your medical care requires prior authorization
While your dermatologist (or practice staff member) will submit the request for prior authorization to your insurance provider, you can help by doing the following:
Communicate quickly with your dermatologist’s office in a HIPAA-secured and private way: If your dermatologist has a patient portal, set up your account if you haven’t already done this.
Avoid delays in your care: The AAD recommends after four business days, if you haven’t heard whether your insurance provider approved (or denied) the request for prior authorization, follow up with your dermatologist’s office and your insurance provider.
Make sure you’re following your treatment plan: It can take time to get prior authorization. If your insurance provider approves the request for prior authorization, it can be helpful to log in to your patient portal to review your treatment plan before starting it.
Dermatologists help their patients get the care they need
Dealing with the prior authorization process can be frustrating, confusing, and overwhelming. Dermatologists understand this and work hard to ensure that their patients get the care they need.
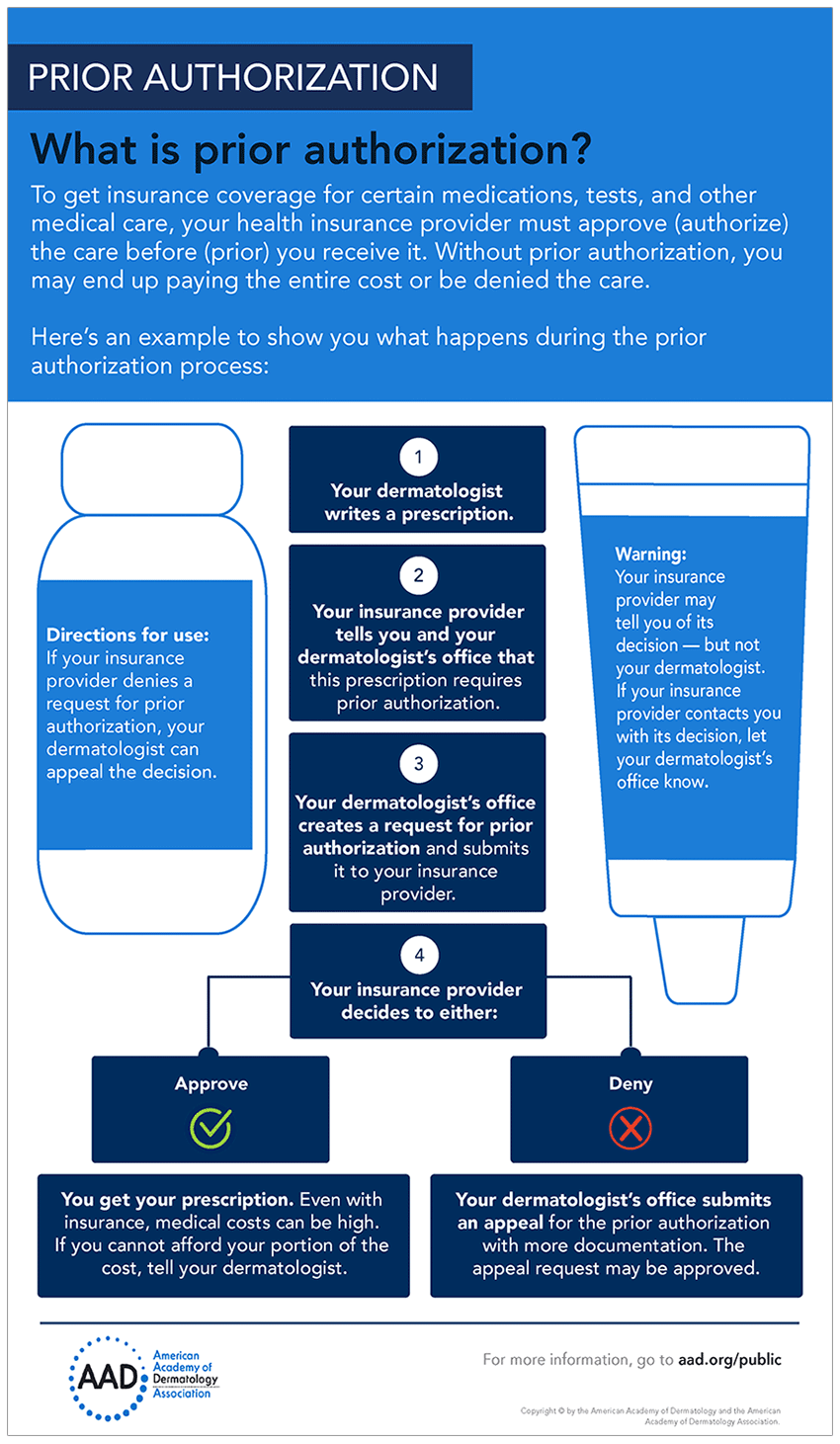
Infographic: What is prior authorization?
This infographic shows the steps during the prior authorization process.
Related AAD resources
Image
Getty Images
References
1Popatia S, Flood KS, et al. “Examining the prior authorization process, patient outcomes, and the impact of a pharmacy intervention: A single-center review.” J Am Acad Dermatol 2019;81:1308-18.
2Ibid.
Written by:
Swapna Bhatia, MPH
Michelle Pizarro, MHA
Reviewed by:
Sanna Ronkainen, MD, FAAD
Shari Lipner, MD, PhD, FAAD
Last updated: 2/3/21
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?