Epidermolysis bullosa: Overview
What exactly is EB?
Epidermolysis bullosa (EB) is a group of rare diseases that cause the skin to blister easily.

Some children develop blisters in the moist tissue that lines the mouth, throat, stomach, intestines, rectum, and other areas of the body. In these areas, the friction caused by swallowing food or having a bowel movement can lead to painful blisters.
The effects that EB has on a child’s life varies considerably. Some children have a mild disease that requires taking precautions to prevent injuries. At the other end of the spectrum, EB can cause lifelong disability that needs ongoing medical care.
Some types of EB are less likely to cause lifelong disability, but any type of EB can cause severe symptoms, as the following descriptions of the different types of EB indicate.
Types of epidermolysis bullosa (EB)
Epidermolysis bullosa simplex (EBS): This is the most common type. In its mildest form, the blisters usually occur only on the hands and feet of a newborn. Later in life, the skin may stop blistering, leaving a teen or adult with thickened, hard skin on the palms and soles.

As the blisters clear, the skin tends to heal without scarring.
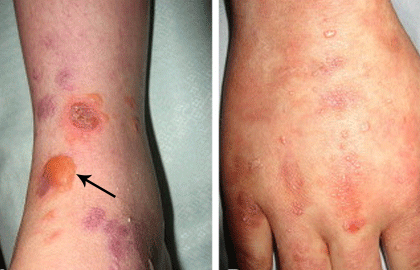
Dystrophic epidermolysis bullosa (DEB): When a child has a mild case of DEB, blisters tends to develop only on the hands, feet, knees, and elbows.
Blistering can also be widespread, causing severe DEB. A baby born with severe DEB, can have widespread blistering and areas of missing skin. Blisters may develop inside the mouth and esophagus, which makes swallowing painful. When this happens, the child may need a feeding tube.
As the blisters heal, scars tend to form. When skin on the fingers or toes repeatedly blisters and scars, the fingers or toes can join together. Repeated blistering and scarring is what caused the child shown in this picture to have fused toes. When the toes join together, walking becomes difficult.

People with DEB can also develop fatal skin cancers. This happens because the skin cancer is much more aggressive, which makes it difficult to treat the cancer successfully.
You can find out what it’s like to live with a severe type of DEB by reading Fragile skin, strong spirit: Jonathan Gionfriddo’s story.
Junctional epidermolysis bullosa (JEB): When JEB is mild, blisters usually develop only on the newborn’s hands, elbows, knees, and feet. The blistering tends to lessen by 2 or 3 months of age.
JEB can also be severe, with blisters developing on large areas of the body or digestive tract.
As blisters heal, scars appear. This can cause the toes or fingers to join together, but taking precautions can reduce the risk of this happening.

Kindler syndrome: This is a very rare type of EB. Only about 100 cases of Kindler syndrome have been reported since 1954. The largest number of known cases occurred within a tribe that lives in rural Panama.
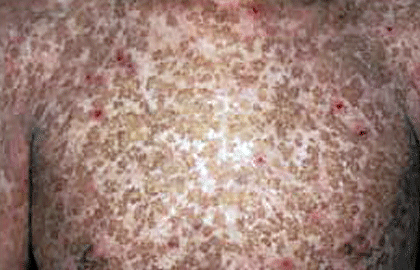
At birth, the skin blisters easily and is extremely sensitive to the sun. As the child grows, the blistering and sensitivity to the sun will lessen. As these diminish, a skin condition called poikiloderma appears. It causes dark patches on the skin, so the skin starts to look a lot like that shown in this picture.
At first, the dark patches appear only on skin that gets some sun. After puberty, the dark patches tend to appear everywhere on the skin. By this stage, you may also see visible blood vessels and the skin on the hands and feet tends to thin greatly. The skin also becomes so dry and wrinkled that the hands and feet resemble that of an elderly person’s.
Epidermolysis bullosa acquisita (EBA): Extremely rare, this type of EB differs from the other types. This type of EB is thought to be an autoimmune disease. When someone develops an autoimmune disease, the person’s immune system mistakes a part of the body as foreign and attacks it.
When a person has EBA, the body attacks the body’s collagen, which is found in the skin and throughout the body. This attack leads to blistering.
Unlike the other types of EB, which begin at birth or shortly thereafter, EBA usually begins in one’s 30s or 40s. Blisters tend to develop on the hands, knees, elbows, and ankles. Blisters can also be widespread and form inside the mouth, nose, or eyes.
Researchers are making progress in the treatment of EB
While EB cannot be cured, researchers are making strides in understanding this rare group of diseases. This understanding has led to new treatments that can provide better relief from the symptoms.
You’ll find more information about possible symptoms at, Epidermolysis bullosa: Signs and symptoms.
Images
References
Fine JD, Bruckner-Tuderman L, et al. “Inherited epidermolysis bullosa: Updated recommendations on diagnosis and classification.” J Am Acad Dermatol. 2014;70:1103-26.
Ghosh SK, Bandyopadhyay D, et al. “Kindler’s Syndrome: A case series of three Indian children.” Indian J Dermatol. 2010;55:393-6.
Hilton L. “EB’s great hope: Pediatricians respond to the first successful gene therapy treatment.” Dermatol Times. 2018;39(2):1+.
Penagos H, Jaen M, et al. “Kindler syndrome in native Americans from Panama: Report of 26 cases.” Arch Dermatol. 2004;140:939-44.
Seta V, Aucouturier F, et al. “Comparison of 3 type VII collagen (C7) assays for serologic diagnosis of epidermolysis bullosa acquisita (EBA).” J Am Acad Dermatol. 2016;74:1166-72.
Watkins, J. “Diagnosis, treatment and management of epidermolysis bullosa.” Br J Nurs. 2016 Apr 28;25(8):428-31.
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?