Is that stubborn acne really acne?

Stubborn acne can also be a sign of something serious going on inside your body. To see clearer skin, you’ll need to get that serious condition under control first.
You’ll find pictures along with descriptions of such skin conditions below. If your acne resembles any of these pictures, seeing a dermatologist can help you get the right diagnosis and treatment.
Six skin conditions that can look like acne
Polycystic ovary syndrome (PCOS)
Clues you have more than acne: Women who have PCOS often have acne. They usually have other signs of a hormone problem, such as hair loss on their head, noticeable hair growth on their face, or an area of skin that starts to darken and sometimes thicken. PCOS can also cause irregular periods, sleep apnea, diabetes, heart disease, and other health problems.

If you’re diagnosed with PCOS, you should also be under the care of a doctor who can treat the cysts in your ovaries. You may also need to see other doctors to get treatment for conditions like diabetes or heart disease.
A dermatologist can treat your acne, hair loss, and noticeable hair growth. The darkening skin usually goes away when the disease causing it is treated. The medical name for this darkening skin is acanthosis nigricans.
Related AAD resource
Rosacea

Treatable: Yes. Treatment can clear the acne-like breakouts and help your skin feel better. Rosacea cannot be cured, so you may need ongoing treatment.
Related AAD resource
Keratosis pilaris
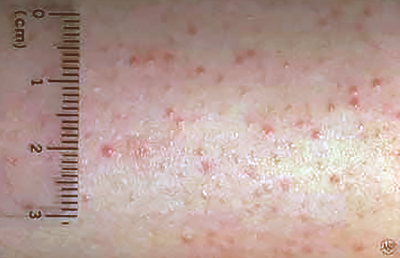
Treatable: These bumps are harmless, so you don’t need to treat them. If the itch, dryness, or appearance bothers you, treatment can help.
Related AAD resource
Hidradenitis suppurativa (HS)

Treatable: Yes. Treatment is important because it can prevent HS from worsening. If HS worsens, the acne-like eruptions can grow deep into the skin and become painful. They can rupture, leaking bloodstained pus onto your clothing. This fluid often has a foul odor.
As the deep bumps heal, scars can form. With repeat outbreaks, the skin often begins to look spongy as tunnel-like tracts form deep in the skin.
Related AAD resource
Perioral dermatitis

Treatable: Yes. Dermatologists recommend treatment. Without it, the dermatitis may last for months or years.
Related AAD resource
Chloracne

The signs and symptoms usually develop 2-4 weeks after you’ve come into contact with toxic chemicals found in insecticides, herbicides, or wood preservatives. Agent Orange was a known cause of chloracne during the Vietnam War.
Treatable: The skin will clear when you stop coming into contact with the chemical that caused the chloracne. The clearing usually happens within 6 months to 3 years.
The skin can also be treated with antibiotics, isotretinoin (a medicine used to treat severe acne), or procedures that dermatologists use to treat other skin conditions.
Dermatologists can help you see clearer skin
If your stubborn acne looks like any of these conditions, seeing a dermatologist can be helpful. A dermatologist can tell you whether it’s stubborn acne or another condition. Your dermatologist can also create a treatment plan for you, whether you have one of these skin conditions that looks like acne or stubborn acne.
Yes, even stubborn acne can be treated successfully. Thanks to advances in acne treatment, virtually everyone can see clearer skin.
Images
Images 1, 4, 5, and 7: Used with permission of the Journal of the American Academy of Dermatology.
(J Am Acad Dermatol 2007;56:S100-2.)
(J Am Acad Dermatol 2010;62:637-45.)
(J Am Acad Dermatol 2015;73:672-90.)
(J Am Acad Dermatol 2016;74:143-70.)
Images 2, 3, 6: Used with permission of the American Academy of Dermatology National Library of Dermatologic Teaching Slides.
References
Alikhan A, Lynch PJ, et al. "Hidradenitis suppurativa: A comprehensive review." J Am Acad Dermatol 2009;60(4):539-61.
Chamlin SL and Lawley LP. “Perioral dermatitis.” In: Fitzpatrick’s Dermatology in General Medicine (seventh edition). McGraw Hill Medical, New York, 2008: 709-12.
Crawford GH, Crawford GH, et al. “Rosacea: I. Etiology, pathogenesis, and subtype classification.” J Am Acad Dermatol. 2004;51(3):327-41.
Nedorost ST. “Medical Pearl: The evaluation of perioral dermatitis: Use of an extended patch test series.” J Am Acad Dermatol. 2007;56(5 Suppl):S100-2.
Patterson AT, Kaffenberger BH, et al. “Skin diseases associated with Agent Orange and other organochlorine exposures.” J Am Acad Dermatol. 2016;74:143-70.
Schmitt JV, Lima BZ. “Keratosis pilaris and prevalence of acne vulgaris: a cross-sectional study.” An Bras Dermatol. 2014 Jan-Feb; 89(1):91–5.
Sood A and Taylor JS, “Occupational noneczematous skin disease due to biologic, physical, and chemical agents.” In: Fitzpatrick’s Dermatology in General Medicine (seventh edition). McGraw Hill Medical, New York, 2008: 702.
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?