Diabetes: 10 warning signs that can appear on your skin
Diabetes can affect many parts of your body, including your skin. When diabetes affects the skin, it could mean that:
You have undiagnosed diabetes or pre-diabetes.
Your treatment for diabetes needs to be adjusted.
It’s time to talk with your doctor if you notice any of these warning signs on your skin.
1. Shin spots
This skin condition is common in people who have diabetes. The medical name for shin spots is diabetic dermopathy. You may also hear people refer to this condition as spotted leg syndrome.
When this condition begins, you usually see round or oval spots, which often develop on the shins. The spots may be brown or reddish brown in color.
Early on, these spots often feel scaly. As they flatten out, they can cause small dents in the skin.
Diabetic dermopathy
Because these spots are often brown and cause no symptoms like itch or pain, many people mistake them for age spots.

Unlike age spots, these spots often start to fade after diabetes is well-controlled, usually within 18 to 24 months. Diabetic dermopathy can also stay on the skin indefinitely.
While these spots are harmless, anyone who develops them and hasn’t been diagnosed with diabetes should be tested.
If you have diabetes, tell your doctor about these spots. Some people who have diabetes and shin spots have a higher risk of developing complications from diabetes like neuropathy, which is nerve damage that can lead to weakness, numbness, and pain.
Take action
Tell your doctor about these spots.
If your diabetes isn’t well controlled, work with your doctor to gain better control.
2. Darker area of skin that feels like velvet
A dark patch (or band) of velvety skin on your neck, armpit, groin, or elsewhere could be a sign of pre-diabetes. The medical name for the condition that causes this velvety skin is acanthosis nigricans.
Acanthosis nigricans on the neck
Often developing on the back of the neck, this condition may be the first sign that someone has diabetes or prediabetes.

Take action
Get tested for diabetes.
3. Hard, thickening skin
If you have diabetes, hard, thick, and swollen-looking skin can develop, even when diabetes is well controlled. The medical name for this condition is scleredema diabeticorum.
Often developing on the upper back, the skin thickens and tightens slowly over months or years. This condition can also occur on the shoulders, neck, or elsewhere, but never on the hands or feet.
Scleredema diabeticorum
Some people have discoloration where the skin is hard and thickening.
While the skin hardens and thickens, the condition is painless.

Take action
Tell your doctor about thickening skin. Getting better control of your diabetes may bring relief.
4. Open sores and wounds
Having high blood sugar (glucose) for a long time can lead to poor circulation and nerve damage. You may have developed these if you’ve had uncontrolled (or poorly controlled) diabetes for a long time.
Poor circulation and nerve damage can make it hard for your body to heal wounds. This is especially true on the feet. The open wounds are called diabetic ulcers.
If you have diabetes, check your feet every day for sores and open wounds
If you see a sore, cut, open wound, swelling, discoloration, or other change, contact your doctor right away.

Take action
Get immediate medical care for an open sore or wound.
Work with your doctor to make sure your diabetes is well controlled.
5. Outbreak of small bumps
Uncontrolled diabetes can cause extremely high levels of triglycerides, a type of fat that circulates in the blood. If this happens, you can develop a skin condition called eruptive xanthomatosis.
Eruptive xanthomatosis
If you have undiagnosed diabetes or diabetes that is not well controlled, these bumps can appear on your skin suddenly.

After the bumps appear, they soon develop a yellowish color in lighter skin tones. If you have a darker skin tone, you may see a grayish color with a yellowish hue beneath. You’ll usually find these bumps on the buttocks, thighs, crooks of the elbows, or knees. They can form anywhere though. No matter where they form, they are usually tender and itchy.
Once the diabetes is well-controlled, the bumps tend to go away.
Take action
Tell your doctor about the bumps because this skin condition can develop when you have uncontrolled diabetes.
Talk with your doctor about how to better control your diabetes.
6. Yellowish, smooth bumps or patch(es) on and around your eyelids
These bumps and patches develop when you have high levels of fat in your blood, which can be a sign that you have poorly controlled diabetes. The medical name for this condition is xanthelasma.
Regardless of your skin tone, these bumps and patches look yellowish or yellowish orange in color.
Xanthelasma
The yellowish bumps and patches usually appear in about the same place on (or around) both eyelids. These bumps and patches can feel soft or somewhat hard.

Take action
Tell your doctor about the yellowish bumps or patches around your eyes.
If you have diabetes, talk with your doctor about how to better control this condition. Controlling diabetes may clear the bumps and patches.
7. Infections
Diabetes weakens your immune system, which reduces your body’s ability to fight off harmful germs and increases your risk of developing infections. It's common to develop infections in the mouth like oral thrush or in the vagina like a yeast infection.
Do you get several yeast infections each year?
Ask your doctor if you might have diabetes or pre-diabetes.

Take action
Get immediate treatment for the infection.
Tell your doctor if you have frequent yeast infections. You could have undiagnosed diabetes.
If you’ve been diagnosed with diabetes, you may need better control of it.
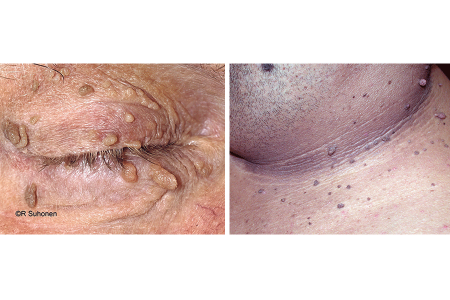
8. Skin tags
Many people have skin tags, which are harmless growths that can appear anywhere on the skin. Sometimes, skin tags are firmly fixed to the skin. You may also see ones that dangle from a stalk. The medical name for these growths is acrochordons.
While skin tags can develop anywhere on the skin, they are most common on the eyelids, neck, armpit, and groin.
Skin tags
While harmless, having many skin tags may be a sign that you have type 2 diabetes.
Take action
If you have many skin tags on your skin:
Ask your doctor if you should get tested for diabetes.
If you have diabetes, ask your doctor if you need better control of it.
9. Cluster of small bumps or a raised patch
Whether this skin condition is associated with diabetes is controversial. We know that most people who have granuloma annulare do not have diabetes.
Several studies, however, have found this skin condition in patients who have diabetes. One such study found that people with diabetes were most likely to have granuloma annulare over large areas of skin and that the bumps came and went. Another study concluded that people who have granuloma annulare that comes and goes should be tested for diabetes.
Granuloma annulare
This skin condition causes bumps and patches that may be skin colored, red, pink, or bluish purple.

Take action
Let your doctor know if you have small bumps on your skin, making sure to tell your doctor if the bumps come and go.
10. Yellow, reddish, brown, or purplish patches on your skin
When this condition begins, you’ll often see one or a few reddish-brown spots on your shins if you have a lighter skin tone. People with darker skin tones often see purplish spots. These spots aren’t itchy or painful. The medical name for this condition is necrobiosis lipoidica.
These spots grow slowly, becoming one or more patches that may be yellow, reddish, brown, or purplish. In the center, you may see waxy skin that is thinning, blood vessels, or both.
Necrobiosis lipoidica on a person’s shins
The lighter areas in the reddish patches are waxy-feeling skin.

Take action
Get tested for diabetes if you have not been diagnosed.
Work with your doctor to better control your diabetes.
See a dermatologist about your skin. Necrobiosis lipoidica is harmless, but it can lead to complications.
When to see a dermatologist
Diabetes can cause skin problems. Most of these skin problems are harmless, but even a minor one can become serious if you have diabetes. A board-certified dermatologist can recognize skin problems due to diabetes and help you manage them.
Are all dermatologists board certified?
No. See what it takes to become board certified.
Images
Images 1, 2, 6, 8, 9, 11, 12, 13, 14: Reproduced with permission from ©DermNet www.dermnetnz.org 2023.
Image 3, 4: Used with permission of the Journal of the American Academy of Dermatology:
J Am Acad Dermatol 2007;57:502-8.
J Am Acad Dermatol 2014;71:e99-e101.
Images 5, 10: Getty Images
Image 7: Used with permission of the American Academy of Dermatology National Library of Dermatologic Teaching Slides.
References
Centers for Disease Control and Prevention. “Diabetes and your feet.” Last updated 4/11/2023. Last accessed 11/28/2023.
Cohen Sabban, EN. “Cutaneous manifestations of diabetes mellitus from A to Z.” Focus session presented at: 74th Annual Meeting of the American Academy of Dermatology; March 4-8, 2016; Washington D.C.
Duff M, Demidova O, et al. “Cutaneous manifestations of diabetes mellitus.” Clinical Diabetes. 2015;33:40-8.Lima AL, Illing T, et al. “Cutaneous manifestations of diabetes mellitus: A review.” Am J Clin Dermatol. 2017 Aug;18(4):541-53.
Martín C, Requena L, et al. “Scleredema diabeticorum in a patient with type 2 diabetes mellitus.” Case Rep Endocrinol. 2011;2011:560273.
McKinley-Grant L, Dronavalli S, et al. “Cutaneous manifestations of systemic disease.” In: Taylor and Kelly’s Dermatology for Skin of Color. (second edition). McGraw Hill, USA, 2016:479-85.
Morgan AJ and Schwartz RA. “Diabetic dermopathy: A subtle sign with grave implications.” J Am Acad Dermatol. 2008;58:447-51.
Pereira M, Pinheiro RR, et al. “Scleredema diabeticorum.” Dermatol Reports. 2022 Nov 21;14(4):9477.
Vangara SS, Klingbeil KD, et al. “Severe hypertriglyceridemia presenting as eruptive xanthomatosis.” J Family Med Prim Care. 2018 Jan-Feb;7(1):267-70.
Written by:
Paula Ludmann, MS
Reviewed by:
Brendan Camp, MD, FAAD
Amanda Friedrichs, MD, FAAD
William D. James, MD, FAAD
Omolara Olowoyeye, MD, FAAD
Last updated: 5/22/24
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?
