BCC mockup
Basal cell carcinoma
What is basal cell carcinoma?
Basal cell carcinoma (BCC) is the most common type of skin cancer. When found early, BCC is highly treatable. Board-certified dermatologists have expertise in diagnosing and treating this skin cancer.
Is basal cell carcinoma contagious? No.
Basal cell carcinoma is the most common type of cancer
If you’ve been diagnosed with basal cell carcinoma (BCC), you have plenty of company. Basal cell carcinoma is the most common type of skin cancer. It’s also the most common type of cancer. Doctors diagnose millions of people with basal cell carcinoma every year.
Reviewed by:
Carrie L. Kovarik, MD, FAAD
Natalie H. Matthews, MD, FAAD
Darrell S. Rigel, MD, FAAD
Last updated: 4/28/23
Dermatologist examining patient for signs of skin cancer
You have a greater risk of developing this skin cancer if you have a lighter skin tone and seldom protected your skin from the sun throughout your life or used tanning beds.

People of all skin tones develop basal cell carcinoma. However, people who have light skin that rarely tans and tends to freckle, red or blond hair, and light-colored eyes have a greater risk of developing this skin cancer.
Before basal cell carcinoma develops, people with lighter skin tones often notice signs of sun damage on their skin, such as age spots, patches of discolored skin, and deep wrinkles. These signs can develop years before cancer.
Is basal cell carcinoma serious?
For most people, basal cell carcinoma is not life-threatening. This skin cancer tends to grow slowly. It seldom spreads to another part of the body. Even so, treatment is important.
Over time, basal cell carcinoma can grow wide and deep. It can spread deeply into the skin, wrap around nerves and blood vessels, and invade muscles and bone. When the cancer grows deep, it can change the way you look. For some people, this can be disfiguring.
When found early, this skin cancer is highly treatable. An early basal cell carcinoma can often be removed during an appointment with your dermatologist.
One common sign is a slowly growing, non-healing spot that sometimes bleeds. Basal cell carcinoma can also appear on the skin in other ways.
What are the signs and symptoms of basal cell carcinoma?
Basal cell carcinoma (BCC) is a type of skin cancer that can show up on the skin in many ways. Sometimes, it can be mistaken for a harmless pimple, scar, or sore. Most basal cell carcinoma's grow slowly.
A common sign of basal cell carcinoma
This skin cancer often develops on the head or neck and looks like a shiny, raised, and round growth.

To help you spot basal cell carcinoma before it grows deep into your skin, dermatologists share these 7 warning signs that could be easily missed.
If you find any of the following signs on your skin, see a board-certified dermatologist. Board-certified dermatologists know how to tell the difference between something small and something major.
7 warning signs of basal cell carcinoma that you could mistake as harmless
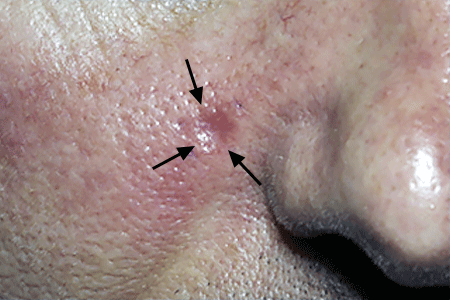
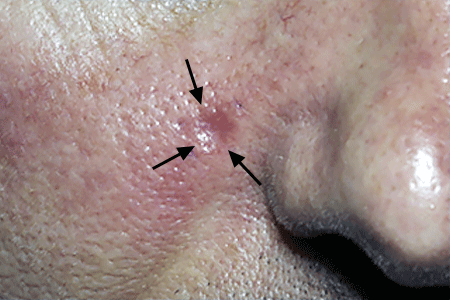
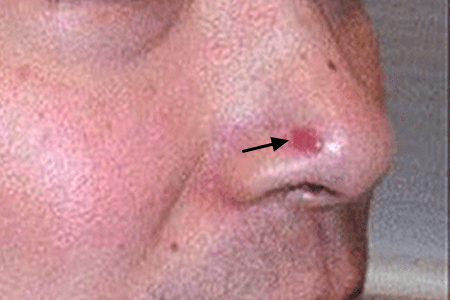
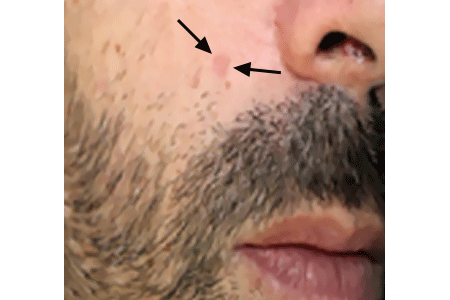
Warning sign: A pink or reddish growth that dips in the center
A pink or reddish growth that dips in the center
The basal cell carcinoma on this patient’s cheek could be mistaken for a minor skin injury.
Warning sign: A growth or scaly area of skin on or near the ear
A growth or scaly area of skin on or near the ear
Basal cell carcinoma often develops on or near an ear. Both the basal cell carcinoma next to a Black woman's ear and the one (circled in purple) next to a white man's ear could be mistaken for a minor skin injury.

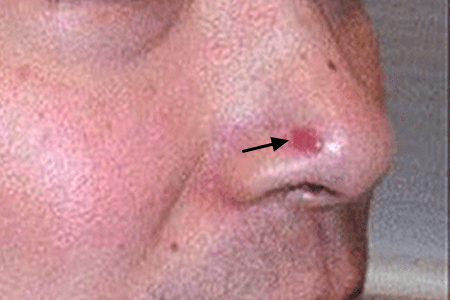
Warning sign: A sore that doesn't heal (or heals and returns) and may bleed, ooze, or crust over
A sore that doesn't heal, or heals and returns
This patient mistook the basal cell carcinoma on his nose for a non-healing pimple.
Warning sign: A scaly, slightly raised patch of irritated skin, which could be red, pink, or another color
A scaly, slightly raised area of irritated skin
This basal cell carcinoma could be mistaken for an area of dry, irritated skin.

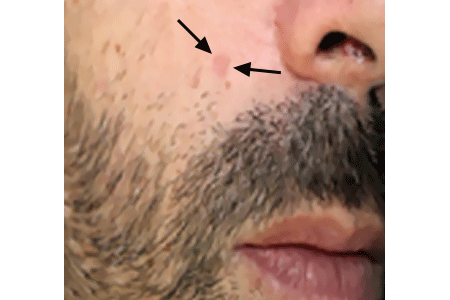
Warning sign: A round growth that may be pink, red, brown, black, tan, or the same color as your skin
A round growth that may be same color as your skin
Would you recognize this as a skin cancer, or would you dismiss it as a harmless growth on your face?

Warning sign: A spot on the skin that feels a bit scaly
A spot on the skin that feels a bit scaly or looks like an age spot
This basal cell carcinoma could easily be mistaken for an age spot, which is why it’s so important to have a dermatologist examine your skin before you treat an age spot.
Warning sign: A scar-like mark on your skin that may be white, yellow, or skin-colored and waxy. The affected skin may look shiny, and the surrounding skin often feels tight.
A scar-like mark on your skin that may be skin-colored or waxy
Appearing on an elderly woman’s skin, this basal cell carcinoma could easily have been mistaken for a scar.

More pictures of basal cell carcinoma
While the above pictures show you some common ways that basal cell carcinoma can appear on the skin, this skin cancer can show up in other ways, as the following pictures illustrate.
Scaly patch with an area of normal-looking skin
On the trunk, basal cell carcinoma may look like a scaly patch with a spot of normal-looking skin in the center and a slightly raised border, as shown here.

Basal cell carcinoma can be lighter in some areas and darker in others
While basal cell carcinoma tends to be one color, it can be lighter in some areas and darker in others, as shown here.

Basal cell carcinoma can be brown
Most basal cell carcinoma are red or pink; however, this skin cancer can be brown, black, blue, gray, the same color as your skin, white, or yellowish.

Basal cell carcinoma can look like a group of shiny bumps
Basal cell carcinoma can look like a group of small, shiny bumps that feel smooth to the touch.

Basal cell carcinoma can look like a wart or a sore
The basal cell carcinoma on this patient’s lower eyelid looks like a wart (spot just below the eyelid marked with an ⁕) in one area and a sore (area on the eyelid marked with two ⁕⁕) in another area.

What color is basal cell carcinoma?
This skin cancer tends to be one color, but the color can vary from one basal cell carcinoma to the next. This cancer may be:
Red or pink (most common)
Brown, black, blue, gray, or show flecks of these colors
The same color as your skin
Yellowish
White
Does basal cell carcinoma hurt?
For many people, the only sign of this skin cancer is a slow-growing bump, sore-like growth, or rough-feeling area on their skin. However, some people develop symptoms where they have this skin cancer.
Symptoms include:
Numbness
A pins-and-needles sensation
Extreme sensitivity
Itching
How do people find basal cell carcinoma on their skin?
Many people find it when they notice a spot, lump, or scaly area on their skin that is growing or feels different from the rest of their skin. If you notice any spot on your skin that is growing, bleeding, or changing in any way, see a board-certified dermatologist. These doctors have the most training and experience in diagnosing skin cancer.
To find skin cancer early, dermatologists recommend that everyone check their own skin with a skin self-exam. This is especially important for people who have a higher risk of developing basal cell carcinoma.
What causes basal cell carcinoma?
The cause of basal cell carcinoma (BCC), the most common type of skin cancer, is well known. Most people develop it because their skin has been badly damaged by ultraviolet (UV) light from:
The sun
Indoor tanning equipment (such as tanning beds or sunlamps)
Both the sun and indoor tanning
People who have lighter skin tones have a higher risk of developing UV-damaged skin.
If you use a tanning bed, you have a higher risk of developing skin cancer
Indoor tanning can increase your risk of developing basal cell carcinoma by 24%¹.

How can UV light cause skin cancer?
Every time UV light hits our skin, it can damage some of the DNA inside our skin’s cells. The body tries to repair this damage.
As UV light from the sun, indoor tanning equipment, or both, continues to hit our skin, the damage builds up. Eventually, it becomes too much for the body to repair. When the body cannot repair the damage, changes called mutations develop. When the mutations build up in the skin, we get skin cancer.
The type of skin cancer we get depends on where the mutations develop in the skin. Basal cells are found deep inside the first layer of our skin, so we get basal cell carcinoma when mutations develop inside these cells.
Do some people have a higher risk of getting basal cell carcinoma?
Yes. The main risk factor (anything that increases your risk of getting a disease) for getting this skin cancer is:
UV-damaged skin, caused by the sun or tanning beds: Each time you go outdoors without protecting your skin from the sun or use a tanning bed, you increase your risk of getting skin cancer.
There are other risk factors for basal cell carcinoma, which include:
Lighter skin tone: This skin cancer develops in skin damaged by UV light, and skin is more easily damaged by UV light if you have a light skin tone and one or more of the following:
Sunburns: If you’ve had sunburns, especially blistering ones in your youth, you have a higher risk of developing this skin cancer.
Live in an area with intense sunlight or the mountains: Living in an area that gets intense sunlight year-round, such as Florida or California, increases your risk of getting skin cancer. People who live at a high altitude also have an increased risk.
Your work: People in certain occupations have a higher risk of developing this skin cancer. For example, studies have found that people who work outdoors have an increased risk when compared to people who work indoors. If you work in one of the following occupations, you may have a higher risk of developing basal cell carcinoma:
- Asphalter
- Farmer, park ranger, and other outdoor worker
- Roofer
- Military service (veterans and active duty)
- Pilot or flight crew
- Welder (metal arc)
Previous skin cancer: If you’ve had any type of skin cancer, you have a greater risk of getting another one.
Weakened immune system: Anything that weakens your immune system increases your risk of getting this skin cancer. In fact, basal cell carcinoma is one of the cancers most likely to develop when the immune system weakens.
Some medical conditions: If you have one of the following medical conditions, you have an increased risk of developing basal cell carcinoma. Some people who have one of these conditions develop hundreds of skin cancers.
100+ PUVA sessions: Used to treat psoriasis and some other conditions that affect the skin, this therapy involves taking a medication called psoralen, which makes your skin more sensitive to UV light. After the medication takes effect, the skin that needs treatment is exposed to controlled UV light.
X-ray treatments for acne: While no longer used to treat acne, some people received these treatments in their youth.
Dialysis for kidney disease: People who are receiving dialysis have a much greater risk of developing basal cell carcinoma.
Arsenic in your food or water: Many researchers have found that the more arsenic found in your food or water, the greater your risk of developing basal cell carcinoma.
While having a risk factor for basal cell carcinoma increases your risk of developing it, some people who get this skin cancer don’t have risk factors. People of all colors get this skin cancer, including people of African, Asian, and Latin descent.
Anyone who finds a spot on their skin that is growing, bleeding, or changing in any way should see a board-certified dermatologist. No one knows your skin better than a board-certified dermatologist.
1American Academy of Dermatology. “Indoor tanning fact sheet.” Last updated 6/21/22. Last accessed 4/11/2023.
Treatment
If you find a spot on your skin that you think could be a skin cancer, an accurate diagnosis and treatment are essential. The following explains how dermatologists diagnose and treat the most common type of skin cancer, basal cell carcinoma (BCC).
Dermatologist treating basal cell carcinoma
When found early, basal cell carcinoma is highly treatable.

How dermatologists diagnose basal cell carcinoma
When you see a board-certified dermatologist, your dermatologist will:
Examine your skin carefully
Ask questions about your health, medications, and symptoms
If your dermatologist finds a spot on your skin that could be any type of skin cancer, your dermatologist will first numb the area and then remove all (or part) of it. This can be done during an office visit and is called a skin biopsy. This is a simple procedure, which a dermatologist can quickly, safely, and easily perform.
Having a skin biopsy is the only way to know for sure whether you have any type of skin cancer. After your dermatologist removes the spot, a doctor, such as your dermatologist or a dermatopathologist, will examine it under a high-powered microscope. The doctor is looking for cancer cells.
If the doctor sees cancerous basal cells, the diagnosis is basal cell carcinoma.
After the doctor examines the removed skin under a microscope, the doctor writes a report. Called a biopsy report or a pathology report, this document explains in medical terms what was seen under the microscope.
If the diagnosis is any type of skin cancer, the information in this report will tell your dermatologist the key facts needed to treat the cancer, including:
The type of basal cell carcinoma you have
How deeply the cancer has grown (when possible to tell)
Your dermatologist will carefully consider your health and the findings in the report before choosing how to treat the cancer.
How dermatologists treat basal cell carcinoma
When possible, basal cell carcinoma is treated with a procedure called “surgical removal.” If you have an early basal cell carcinoma, this can often be performed in your dermatologist’s office while you remain awake. The following explains the types of surgical removal used to treat basal cell carcinoma, along with other treatment options.
Surgical removal: Three types of surgical removal are used to treat basal cell carcinoma. The type of surgical removal you receive depends largely on the type of basal cell carcinoma you have, where it’s located, and how deeply it goes.
Here’s what involved with each type of surgical removal:
Excision: Your dermatologist cuts out the skin cancer and an area of normal-looking skin around it. Removing some normal-looking skin helps to remove stray cancer cells.
Mohs (pronounced moes) surgery: On some areas of the body, such as an eyelid or your nose, removing an area of normal-looking skin along with the cancer would cause problems. There’s not enough skin in these areas.
Curettage and electrodesiccation: During this type of surgical removal, your dermatologist first scrapes the basal cell carcinoma from your skin, using a technique called curetting. Then, a procedure called electrodesiccation is used to destroy any remaining cancer cells with heat.
Freezing or light therapy: While surgical removal (described above) is often the preferred way to treat basal cell carcinoma, one of these following procedures may be recommended for some patients.
Freezing: The procedure is called cryosurgery (cry-oh-sur-jer-ee), and it can be performed during an office visit. Cryosurgery involves spraying an extremely cold substance, such as liquid nitrogen, on the basal cell carcinoma to destroy the tumor.
Light therapy: The medical name for this procedure is photodynamic therapy (PDT). It’s a two-part procedure. First, a solution that makes your skin more sensitive to light is applied to the cancer and a bit of skin around it. You’ll sit with this solution on your skin for one to several hours.
Medication applied to the skin: This is a treatment that you would use at home as prescribed. It’s often used before or after another treatment for basal cell carcinoma. When prescribed as the first treatment, applying medication to the skin cancer helps to reduce the size of the cancerous tumor. Applying the medication after having another treatment helps to kill any remaining cancer cells.
For a few patients, this may be the only treatment prescribed.
Two medications that you apply to the skin have been approved by the U.S. Food and Drug Administration (FDA) to treat basal cell carcinoma:
Imiquimod (eh-mick-quie-mod): This medication is usually applied once a day or once every other day for 6 weeks or longer.
5-FU: This medication is usually applied twice a day for 3 to 6 weeks.
As these medications destroy cancer cells, you will likely feel the effects on the treated area. Side effects of these medications include skin redness, swelling, sores, crusting, itching, and tingling sensations.
Radiation treatments: If this is prescribed to treat basal cell carcinoma, you will need to go to a hospital or treatment center for radiation treatments. These are usually given over a period of several weeks.
For some patients, radiation may be the only treatment given. Radiation can also be used as a follow-up treatment for an aggressive basal cell carcinoma to help destroy cancer cells.
Radiation is typically only used to treat this skin cancer in people who are 60 years of age or older.
How is basal cell skin cancer treated when it grows deep or spreads?
While this skin cancer tends to grow slowly, early treatment is recommended. Without treatment, basal cell carcinoma can grow deep, destroying what lies in its way. This can be disfiguring. The medical term for this is advanced basal cell carcinoma.
It’s also possible for basal cell carcinoma to spread to other parts of your body, but this is rare. When the cancer spreads, it typically travels first to the lymph nodes closest to the tumor. From there, it tends to spread through the blood to bones, the lungs, and other parts of the skin. When this skin cancer spreads, it is called metastatic basal cell carcinoma.
For cancer that has grown deep or spread to the closest lymph nodes, treatment may involve:
Surgery to remove the tumor (and cancerous lymph nodes)
Follow-up treatment with radiation to kill any remaining cancer cells
For some patients, medication that works throughout the body may be an option. Medication may also be used to treat cancer that returns after surgery or radiation treatments.
Two such medications have been approved by the U.S. Food and Drug Administration (FDA). Both come in pill form and are taken every day. A patient only stops taking the medication if the cancer starts to grow, or the side effects become too severe.
The two medications are:
Sonidegib (so-nī-deh-gib)
Vismodegib (vis-moe-deh-gib)
In clinical trials, these medications have been shown to stop or slow down the spread of the cancer and shrink the cancerous tumors in some patients.
Your oncologist (doctor who specializes in treating cancer) may talk with you about another medication used to treat advanced basal cell carcinoma. It’s called cemplimab (semi-ply-mab).
Cemplimab may be an option if sonidegib or vismodegib:
Is not right for you
Stops working
Causes side effects that prevent you from continuing to take it
Cemplimab is a type of medication called immunotherapy. This means it works with your immune system to find and destroy cancer cells. When this happens, tumors can shrink.
Cemplimab is given by infusion, so you would go to your oncologist’s office, a hospital, or cancer treatment center to be treated. Patients receive an infusion once every three weeks. You only stop treatment with cemplimab if it stops working or side effects prevent you from continuing with it.
Newer treatments for deep basal cell skin cancers and ones that have spread are being studied in clinical trials. If you have advanced basal cell carcinoma, you may be eligible for one of these trials.
What is the outcome for someone who has basal cell carcinoma?
When found early and treated, this skin cancer can often be removed. However, this skin cancer can return. You also have a higher risk of developing another basal cell carcinoma or other type of skin cancer.
That’s why self-care becomes so important after treatment for basal cell carcinoma.
Self-care
Once you’ve had basal cell carcinoma (BCC), you have a higher risk of developing another skin cancer, including melanoma, the most serious skin cancer.
You’ll have this increased risk for the rest of your life.
To help you reduce this risk and find skin cancer early, dermatologists recommend the following to their patients who have had basal cell carcinoma:
Keep all your dermatology appointments. Your dermatologist will tell you how often you will need to come in. During these appointments, your dermatologist will check you for signs of skin cancer.
Learn how to examine your own skin for signs of skin cancer, and do this as often as your dermatologist recommends. The purpose of the skin self-exam is to find skin cancer early when it’s most treatable.
FIND SKIN CANCER: HOW TO PERFORM A SKIN SELF-EXAM
Regularly checking your skin can help catch skin cancer early, when it’s highly treatable. Follow these tips from board-certified dermatologists to check your skin for signs of skin cancer.
During your skin self-exam, you want to examine all your skin, even places that rarely get sun. You'll also examine your scalp and nails.
Make an appointment to see your dermatologist if you notice a spot on your skin or scalp that:Protect your skin from the sun. While many people feel that the damage has already been done once they develop skin cancer, protecting your skin from the sun has benefits. Sun protection can prevent further damage to your skin and may allow your body to repair some of the existing damage.
Never use a tanning bed or other indoor tanning equipment. Indoor tanning is not safer than the sun.
When you make an appointment to see your dermatologist, be sure to mention that you’ve been treated for skin cancer.
Seek shade when outdoors
After getting basal cell carcinoma, protecting your skin from the sun can reduce your risk of getting another skin cancer.

You’ll find more information about the different types of skin cancer, including the signs and symptoms of each by going to the, Skin Cancer Resource Center.
Image credits
Images (in order of appearance) used with permission of:
Getty Image
The American Academy of Dermatology National Library of Dermatologic Teaching Slides.
J Am Acad Dermatol. 2019;80:303-17.
J Am Acad Dermatol 2006;55:741-60.
J Am Acad Dermatol. 2006;55:741-60.
J Am Acad Dermatol. 2006;55:741-60.
JAAD Case Rep. 2018; Jun 23;4(6):599-601.
J Am Acad Dermatol. 2019;80:303-17.
JAAD Case Rep. 2018; Jun 23;4(6):599-601.
The American Academy of Dermatology National Library of Dermatologic Teaching Slides.
J Am Acad Dermatol 2006;55:741-60.
J Am Acad Dermatol. 2019;80:303-17.
The American Academy of Dermatology National Library of Dermatologic Teaching Slides.
The American Academy of Dermatology National Library of Dermatologic Teaching Slides.
J Am Acad Dermatol. 2019;80:303-17.
References
Cameron MC, Lee E, et al. “Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations.” J Am Acad Dermatol 2019;80:303-17.
Gloster HM, Neal K. “Skin cancer in skin of color.” J Am Acad Dermatol 2006;55:741-60.
Nouri K, Ballard CJ, et al. “Basal cell carcinoma.” In: Nouri K, et al. Skin Cancer. McGraw Hill Medical, China, 2008: 61-81.
Cameron MC, Lee E, et al. “Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations.” J Am Acad Dermatol 2019;80:303-17.
Nouri K, Ballard CJ, et al. “Basal cell carcinoma.” In: Nouri K, et al. Skin Cancer. McGraw Hill Medical, China, 2008: 61-81.
American Academy of Dermatology. Media Fact Sheet: Indoor Tanning. Last accessed February 8, 2019.
Bichakjian CK, Armstrong A, et al. “Guidelines of care for the management of basal cell carcinoma.” J Am Acad Dermatol 2018;78:540-59.
Bichakjian CK, Olencki T, et al. “Basal cell skin cancer, Version 1.2016, NCCN Clinical Practice Guidelines in Oncology.” J Natl Compr Canc Netw. 2016;14(5):574-97.
Cameron MC, Lee E, et al. “Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations.” J Am Acad Dermatol 2019;80:303-17.
Ferrucci LM, Cartmel B, et al. “Indoor tanning and risk of early-onset basal cell carcinoma.” J Am Acad Dermatol 2012;67:552-62.
Heltoft, K.N., Slagor, R.M., Agner, T. et al. “Metal arc welding and the risk of skin cancer.” Int Arch Occup Environ Health 90, 873-81.
Margosian E. “Occupational associations of skin cancer.” Dermatol World. 2023;33(3):26-32.
Nouri K, Ballard CJ, et al. “Basal cell carcinoma.” In: Nouri K, et al. Skin Cancer. McGraw Hill Medical, China, 2008: 61-81.
Schmitt J, Haufe E, et al. “Occupational UV-exposure is a major risk factor for basal cell carcinoma: Results of the population-based case-control study FB-181.” J Occup Environ Med. 2018 Jan;60(1):36-43.
Cameron MC, Lee E, et al. “Basal cell carcinoma Contemporary approaches to diagnosis, treatment, and prevention.” J Am Acad Dermatol 2019;80:321-39.
Nouri K, Ballard CJ, et al. “Basal cell carcinoma.” In: Nouri K, et al. Skin Cancer. McGraw Hill Medical, China, 2008: 61-81.
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?